The Conference on Inflammation and Tissue homeostasis jointly organised by IFOM and inStem was an international meeting aimed at advancing our understanding of biology at the intersection of basic science and clinical settings for diseases.
When looking at a minor wound, we are quite unaware of the incredibly complex series of events occurring to heal the wound and bring the skin back to its normal condition. This involves a process known as inflammation, which is a first-line defence against any assault on our bodies. Inflammation is followed by other events such as the death of damaged cells and the regrowth of healthy tissue to restore skin in a process called homeostasis. However, when the intricate balances in inflammation and repair go wrong, the body develops problems in the form of conditions like allergies or as diseases like cancer.
A conference recently hosted at the Institute of Stem Cell Biology and Regenerative Medicine (inStem), Bangalore, from 3rd to 5th February 2016, aimed to highlight ongoing global research on the various roles of inflammation and tissue homeostasis in a wide variety of conditions – from normal wound healing and aging, to cellular movement and cancer. The meeting, titled ‘Conference on inflammation and Tissue Homeostasis’ was jointly organised by inStem and IFOM (the FIRC Institute of Molecular Oncology is an Italian non-profit research centre supported by FIRC, the Italian Foundation for Cancer Research), located in Milan.
The meeting is one in a series of initiatives that the inStem-IFOM collaboration has organised to highlight their joint efforts to advance our understanding of biology at the intersection of basic science and clinical settings for diseases such as cancer. This partnership was officially inaugurated with the establishment of the IFOM-inStem Joint Research Laboratory based in Bangalore, India. The two institutes aspire to combine the complementary strengths of their world-class facilities in creating solutions to some of the world’s most intractable biomedical problems. The meeting organized this February aimed to create new, and further expand existing collaborations between international researchers with those in India to pursue questions of mutual interest.
The questions tackled at the conference included: why must one understand the nitty-gritty details of cell signalling to help cure lethal septic conditions? How does diabetes affect the blood vessels, and hence cardio-vascular diseases in Indian populations? How could studying cell movement help in understanding cancer? These brief overviews of selected talks will attempt to covey the tone of the vast variety of interconnected subjects discussed at the meeting.
Vishva M. Dixit: Gasdermin-D mediates LPS-induced non-canonical inflammasome signalling downstream of caspase-11
Lethal sepsis, colloquially known as ‘blood poisoning’, is an inflammatory reaction to an infection that encompasses the whole body and damages even normal tissues and organs. The condition kills nearly 6 million people world-wide due to limited treatment options. Lethal sepsis is highly variable in the nature of its presentation, and the processes that drive this inflammatory condition are not well known – a fact that makes understanding inflammatory processes an important area of research.
Inflammation is a process mediated by the formation of a large multi-protein complex called an ‘inflammasome’. To date, two distinct types of inflammasomes have been described – the first, known as ‘canonical’ inflammasomes, are well-known to be activated when the body prepares a defence against infections, or mounts an allergic reaction. The ‘non-canonical’ inflammasomes, however, are formed specifically in response to sugars (LPS) found on the surfaces of bacteria and is known to cause lethal sepsis. Dr. Vishva Dixit and his colleagues at the biotechnology company Genentech in San Francisco, California, were key discoverers of this ‘non-canonical’ inflammatory signalling pathway.
In a fascinating talk that extended their previous research, Dr. Dixit described the logic and experiments that led to the uncovering of a crucial molecular player in the ‘non-canonical’ inflammatory pathway – the Gasdermin-D protein. In their attempts to elucidate inflammatory signalling pathways, Dr. Dixit’s team discovered a mouse that seemed to have an intact immune system, but was oddly resistant to LPS induced sepsis. An intensive genetic analysis of this mutant mouse strain pointed to the Gasdermin-D gene as carrying the candidate mutation in these mice. However, this discovery left the researchers baffled, since there was virtually nothing known about the protein.
Dr. Dixit’s group deduced that the mutant mice’s resistance to LPS-induced sepsis was likely due to the role played by Gasdermin-D in the ‘non-canonical’ pathway. This conjecture was found to be true when the Gasdermin-D protein was ascertained to be a substrate for caspase-11, a protease in the ‘non-canonical’ inflammasome pathway. Gasdermin-D cleaved by caspase-11 was found to create a powerful downstream mediator of inflammation. Dr. Dixit concluded his talk with the hypothesis that the Gasdermin-family of proteins were a possible family of ‘assassin proteins’ in view of the rapid cell-death induced by Gasdermin-D after its cleavage by caspase-11.
Rekha Samuel: Placental pericyte and endothelial cell cross-talk in gestational diabetes mellitus
Diabetes mellitus is one of the most widespread diseases afflicting the Indian population. It is a condition where blood sugar levels are abnormally high over extended periods of time, mainly due to a lack of the hormone insulin (Type 1 diabetes) or other causes that make cells resistant to the action of insulin (Type 2 diabetes). A third type of diabetes, known as gestational diabetes (GDM), occurs temporarily in pregnant women who have had no previous history of diabetes. Despite the prevalence of this condition, much is unknown about the unique characteristics presented by Indian diabetic patients, especially those involving the blood vessels – the veins, arteries and capillaries – of the human body.
Dr. Rekha Samuel from the Centre for Stem Cell Research (CSCR at the Christian Medical College, Vellore) began an absorbing seminar by explaining that Indian diabetics often have major problems in blood vessels that can lead to complications such as retinopathy (impaired retinal function leading to vision loss). In her efforts to understand how diabetes affects blood vessels, Dr. Samuel and her team have turned to using the placenta as a model system – mainly because the organ is relatively easily available and has a high density of blood vessels. Currently, Dr. Samuel’s team is focussed on detecting and understanding the changes to the smallest components of blood vessels – the capillaries – whose walls are made of two types of cells known as endothelial cells and pericytes.
The group’s findings indicate that women who experienced gestational diabetes, have placentas with blood vessels that look distinctly different from normal placentas. These diabetic placentas have a unique ‘GDM phenotype’, which includes the presence of angiomatous lesions not commonly seen in healthy placentas. Striking ultrastructural examinations revealed abnormalities of pericytes such as pericyte ghosts that are remarkably similar to those seen in diabetic retinopathies. Since pericytes are essential for the development and maintenance of blood vessels (by providing a perivascular support to endothelial cells and promoting their maturation), their loss is the likely cause of the lesions observed.
Growth experiments on foetal stem cells from GDM placentas also showed that such cells had higher death rates, and formed fewer pericytes. The results from Dr. Samuel’s work indicate that GDM is very likely to affect blood vessel growth in the developing foetus and could influence the susceptibility of an unborn child to diabetes-related conditions in the future. Dr. Samuel wrapped up her talk with the hope that her work would also lead to the generation of a model system within which diabetic retinopathy can be studied.
Giorgio Scita: Endocytic control of cellular plasticity and mechanics
One of the major problems in battling cancer arises due to the ability of cancer cells to undergo a process called ‘metastasis’. What happens in metastasis, is that individual cancer cells or small groups of them leave the main mass of the cancer and disseminate into other parts of the body. This causes a ‘seeding’ of cancerous cells throughout the body that leads to secondary tumours in once-healthy tissues, and a sharp decline in the prognosis for recovery. The talk on cellular plasticity and mechanics by Dr. Giorgio Scita (IFOM, Milan) was a captivating mix of physics, engineering and biology that explored how cells can move and how this is important in the context of metastasis.
Cells within our body can exhibit various forms of movement – collective motion in sheets, streaming motions to squeeze through gaps and single amoeboid movements are a few examples. When migrating, monolayers of cells move in a steady, stream-like manner in a particular direction. Under normal conditions, this fluid form of migration undergoes a transformation where the motions of cells become constrained, and the monolayer takes on a glassy gel-like property – a process called ‘jamming’. Such ‘jamming’ in monolayers is thought to be a property of the forces of tension acting on the cells in the monolayer, since the process can be reversed; and monolayers can be ‘unjammed’ via various physical means such as applying stress.
Dr. Scita and colleagues made the surprising finding that endocytosis, the process by which cells ‘engulf’ surrounding fluids and matter, can affect ‘jamming’ and ‘unjamming’ in cellular migration. Following this logic, investigations revealed that certain endocytic protein levels are sufficient in promoting collective motion in cellular monolayers. The link between cellular migration, ‘unjamming’ and endocytosis is especially important in the context of metastasis, since elevated levels of endocytic factors in breast cancers have been linked to higher instances of metastasis and poor prognosis. Dr. Scita ended his talk by highlighting how a better understanding of the process of ‘unjamming’ in cellular monolayers could help in gaining a clearer picture of the process of metastasis in cancer.
Sara Courtneidge: Invadopodia and podosomes in cell migration and invasion
“I believe that cancer cells don’t do unique things. They simply do a lot of things normal cells do, but at the wrong time and place”, was how Dr. Sara Courtneidge (Oregon Health and Science University, Portland) began her presentation on her team’s work on cellular migration. Dr. Courtneidge’s seminar demonstrated her point clearly, when she began to explain the processes involved in the formation of ‘foot-like’ extensions in certain cells.. The formation of these extensions is mediated by a family of proteins, called Tks, which are also known to be important for normal development in embryos where these foot-like extensions are known as ‘podosomes’. The loss of certain Tks genes leads to neonatal death in mice and severe abnormalities in human infants.
When normal cells such as macrophages (cells that engulf bacteria during an immune response to infection) form podosomes, and help the cell in its immunological duties. Similarly, ‘podosomes’ are also essential for the migration of embryonic stem cells during development, which explains why the loss of Tks genes results in abnormal development and early death in humans and mice.
However, when cancerous cells form such structures as a prelude to their imminent dispersal, they are known as ‘invadopodia’, and their formation is thought to be linked to the function of a Tks gene known as Tks5α. Investigations revealed that elevated levels of Tks5α, if detected in late stages of breast cancers and melanomas, indicated poor prognosis and high metastasis probability. In order to decipher the role of Tks5α in tumour cell growth, Dr. Courtneidge’s team used genetic techniques and novel methods of cell culture to show that this gene is essential for the overall growth of tumours. When the Tks5α gene was deleted from cancer cells and these cells were transplanted into mice, they showed decreased growth, poorer blood vessel formation and smaller tumour formation than tumour cells with the intact Tks5α gene. In conclusion, Dr. Courtneidge hypothesised that invadopodia in cancer cells may also function as signalling structures – affecting not only cellular movement, but also the formation of blood vessels – rather than the simple locomotory organs they are thought to be.
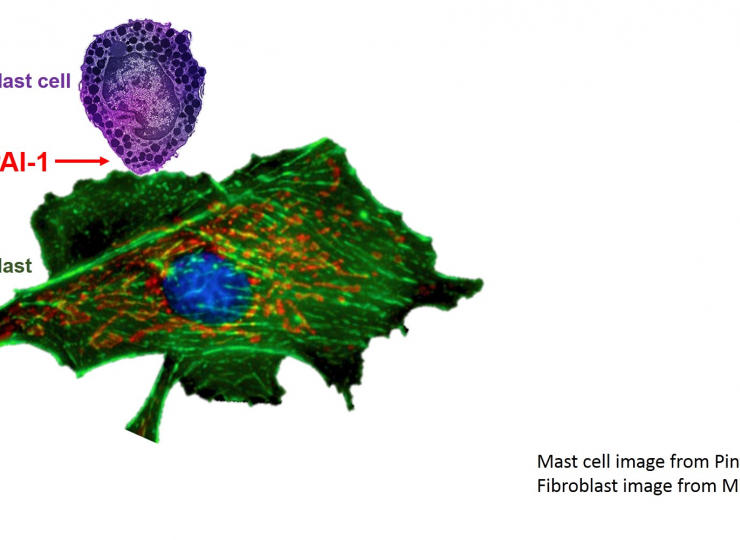
For an enlarged version, please click the image
About IFOM:
IFOM, the FIRC Institute of Molecular Oncology, is a highly technological, non-profit research centre in Italy supported by FIRC, the Italian Foundation for Cancer Research. Research conducted at IFOM aims to understand the molecular processes responsible for the onset and development of cancer. Through strong international approaches, IFOM has fostered partnerships with world-class research institutes in Singapore and India. For more about IFOM, please visit: https://www.ifom.eu/en/
About inStem:
The Institute of Stem Cell Biology and Regenerative Medicine (inStem) is a research institution in Bangalore, India, with a scientific mandate that encompasses the broad area of stem cell and regenerative biology. Research at inStem integrates a wide range of topics within the scope of stem cell biology – from investigations on the fundamental mechanisms that control differentiation and renewal in tissues, to clinical studies on the impact of stem cells during recovery from injuries such as strokes. At inStem, the science is emphasized by collaborative research through cross-disciplinary, multi-pronged approaches that straddle the divide between clinical and laboratory research in stem cell biology. For more information about inStem, please visit: https://www.instem.res.in/
For more about the inStem-IFOM Joint Research Laboratory, please visit: https://www.instem.res.in/ifom